Anemia in Pregnancy
What is it?
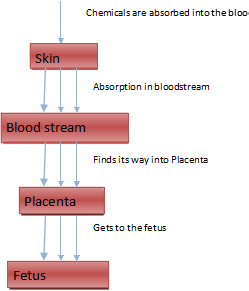
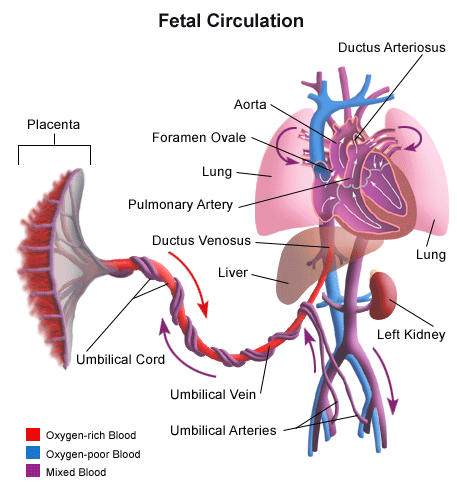
Anemia is the most common nutritional problem affecting pregnant women. Anemia itself is not a diagnosis, but is a sign of a problem; there are multiple etiologies of anemia. In pregnancy one of the most common causes of anemia is that there is an increase in blood volume but less red blood cells are made. This results in a dilutional anemia; note however, your hemoglobin level should not go below 11. There are nutritional causes or anemia as well: the most common nutritional cause of anemia is iron deficiency. Iron is needed to carry oxygen in the blood, and this oxygen then supports the mom and the baby. Anemia in pregnancy is commonly attributed to the deficiency of iron, folate,and vitamin B12. Iron-deficiency anemia is the most commonly observed pregnancy-related anemia affecting about 15% to 25% of all pregnancies.
However, folic-acid deficiency anemia occurs in only about 1% to 5% pregnancies worldwide. Other common causes of anemia include folate and vitamin B12 deficiency, chronic liver disease, HIV, chronic renal disease etc. Symptoms associated with anemia may be maternal tachycardia, shortness of breath, being constantly tired, palpitations, lightheadedness ..unfortunately, these symptoms are also consistent with the normal symptoms experienced by women in pregnancy.
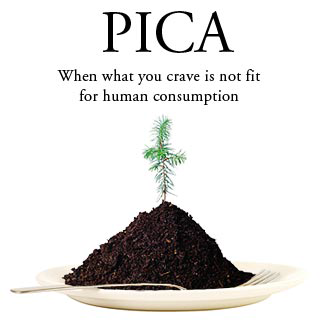
Some women with an underlying anemia during pregnancy, consume large amounts of nonnutritional substances: ice, chalk, corn starch, soil, matches, sand, hair, soap…and other similar textured substances. This is called Pica. The exact etiology why they eat these substances is unknown, however it makes the anemia more severe. I have had many patients who were sent to me with a diagnos i s of severe anemia (Hemoglobin around 6-7). Upon further questioning, i realized these women had pica,. They were consuming 20-30 large glasses of ice daily. Only after they stopped eating the substance did their hemoglobin levels rise, along with large amounts of iron replacement. In some situations, because the patient was so close to delivery, they needed blood transfusions.
Some anemias are due to a genetic error in the hemoglobin, these are called hemoglobinopathies. Examples include, sickle cell disease, thalassemia…etc. If you have anemia, your physician will order an iron level, folate level, vitamin b12 level, haptoglobin and a hemoglobin electrophoresis. These tests will help determine if you have a nutritional deficiency, or a genetic problem, or a problem with increased red blood cell destruction. This will guide your physician to the etiology of your anemia and best treatment for you.

How it affects Pregnancy & Baby?
In studies, severe anemia is associated with adverse fetal outcome, and possible preterm delivery. In these studies, the hemoglobin level was around 4-6. Note however, if your hemoglobin is below 11, you still should have the appropriate workup, and follow treatment if necessary. A low hemoglobin puts you at risk for medical consequences if you have severe bleeding in pregnancy (hemorrhage) or if you are at risk for hemorrhage (if you undergo a cesarean section). For instance you may need a blood transfusion. Genetic causes of anemia such as thalassemia, or sickle cell disease, may place the baby for risks of inheritance. If you have a genetic cause for your anemia, you should see a genetic counsellor during by your pregnancy to ensure you are aware of all potential risks to your baby.
Treatment
The treatment depends on the etiology of your anemia. This usually involves, iron, or vitamin B12, or folate. Iron supplementation is associated with some side effects, most notably constipation, nausea vomiting, and diarrhea. The most effective way to take iron supplements is with orange juice and food, not with milk.
If your etiology is pica, then stopping the offending action (through diet) will usually help, along with supplements. A followup hemoglobin level about 4-6 weeks after initiating treatment will demonstrate improvement. If the anemia is severe, and you
are going to deliver within 1-2 weeks, you may need a blood transfusion, or intravenous iron. Your practitioner will assess the severity of your anemia with the risk delivery.
Although extremely common in pregnancy, anemia is usually recognized early, and once an accurate etiology is determined, anemia can be treated without adversely affecting the pregnancy.
For more helpful pregnancy hints, instructional pregnancy videos, upcoming podcasts and to get more information about the world’s first non-toxic makeup exclusively for pregnant women, please go to www.VSACHARMD.com.
All Rights Reserved, Copyright 2014
No Part of This Post May Be Reproduced Without Expressed Approval from V Sachar MD