Why is Non-toxic, Safe Makeup in Pregnancy Important?
Congratulations!! You are pregnant! This is one of the most exciting and special times in a woman’s life. Now it’s time to plan for a safe pregnancy.
Everybody is concerned about toxins. Pesticides, cigarette smoke, pollution, bisphenol A (BPA), organic, gluten-free…these phrases are thrown at us countless times per day in magazine ads, news reports and commercials.
What about in pregnancy? What should you do? Does it matter?
In 2004, and 2009, two different studies from the Environmental Working Group examined newborn’s blood, and found over 200+ toxins in newborn’s blood! Some of these toxins were pesticides, Bisphenol A, mercury, some are known to cause cancer, and some are known to be neurotoxic. The babies were exposed in utero to these chemicals directly from the mother’s exposure.
Some of these toxins can have an immediate affect, such as low birth weight. But some cause problems later in the child’s life. There is a phenomenon called bioaccumulation,where small amounts of toxin are absorbed, but as the baby grows, these small amounts build up and become toxic to the child.

These toxins can come from multiple sources; food, air, and even makeup.
A healthy environment is important during pregnancy. In a recent study released in February 2013, it was found that pregnant women who were living in cities with higher pollution were more likely to give birth to underweight babies. Clearly, exposure to a high toxin burden, can adversely affect your babies growth.
What about toxin exposure through skin? Is your makeup safe for your pregnancy?
In March 2013 the Safe Cosmetics and Personal Care Products Act was introduced in the US Congress. It aims to ensure that all personal care products are safe by establishing a system to assess the safety of makeup and cosmetic ingredients and to phase out the most harmful substances that are suspected of causing cancer, reproductive harm or other adverse health effects. Toxin exposure in makeup has got the attention of the US Government!
Did you know that there is lead in many brands of makeup in the USA today!The lead content comes from the use of dyes to give color. The FDA tested commonly used lipsticks and reported their findings in this detailed report:
http://www.fda.gov/cosmetics/productandingredientsafety/productinformation/ucm137224.htm
This report will surprise you!! There is no safe level of lead. Lead should not be in any of our products. Even though the individual amounts in each lipstick maybe small, a phenomenon of bioaccumulation occurs. This is when repeated levels of low amounts,build up over time, and can become toxic levels. In pregnancy, lead can be transferred to the fetus as early as the first trimester, and is associated with neurodevelopment delay.
We carefully choose every ingredient to ensure that there is no lead in any of our products.
How can a fetus get exposed to toxins in makeup? This is described as transdermal absorption or across the skin absorption.
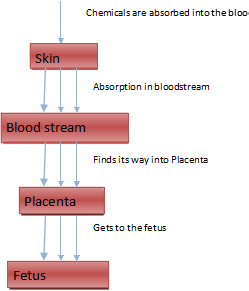
Figure 1: Chemical Absorption by Fetus
After the chemicals pass through the skin, they get absorbed into the bloodstream. The mothers blood directly goes to the baby along with nourishment, oxygen etc. The mother’s blood goes to the placenta which is the interface between the mom and the baby. Nourishment, oxygen and other substances get transferred to the placenta, and then from the placenta to the baby via the umbilical cord.
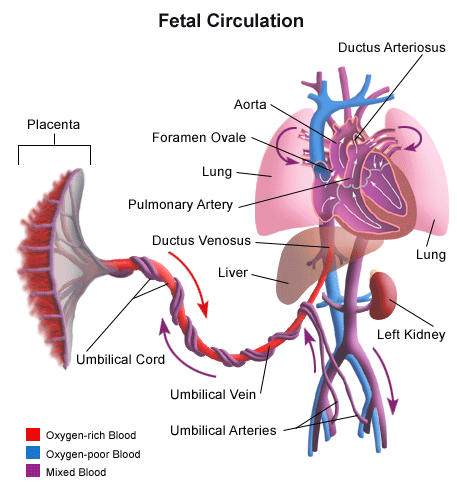
Figure 2: Fetal blood circulation
Chemicals found in cosmetics have been found to affect both the mother and the baby in a number of ways. Most commonly, they interfere with hormonal balance amounting to what is commonly known as endocrine disruption. This can occur in the mother, and the baby. For instance, in pregnancy, exposure to parabens, and phthalates may be associated with reproductive anomalies in the baby later in life. For the mother, prolonged exposure to certain chemicals such as parabens may be associated with breast cancer. The European Union classifies pthalates as a suspected endocrine disruptor on the basis of evidence that it interferes with hormone function, and as toxic to reproduction on the basis that it may cause harm to the unborn child and impair fertility. As well, Health Canada notes evidence suggesting that exposure to phthalates may cause health effects such as liver and kidney failure in young children when products containing phthalates are sucked or chewed for extended periods. Parabens can mimic estrogen, the primary female sex hormone. They have been detected in human breast cancer tissues, suggesting a possible association between parabens in cosmetics and cancer. Parabens may also interfere with male reproductive functions.
You probably have parabens and a number of other toxins in your makeup, and aren’t even aware! Check the labels of your cosmetic products.
Pregnancy is the most important time to protect yourself agains toxin exposure. Limit yourself from pesticides by washing all produce, don’t expose yourself to pollution and cigarette smoke, and try to choose safe makeup.
Now there is a safe makeup alternative for pregnant women. To give women a choice in their makeup, I have created the world’s only safe, non-toxic makeup exclusively for pregnancy. I have removed potential toxins, lead,allergens, and irritants from our ingredients. This is the world’s safest makeup for the mother AND the baby. We feel that our makeup is the best natural, and toxin free makeup that is safe in pregnancy. Go to www.VSACHARMD.com to get more information.