Abnormal Pap Smear in Pregnancy
What is an Abnormal Pap Smear?
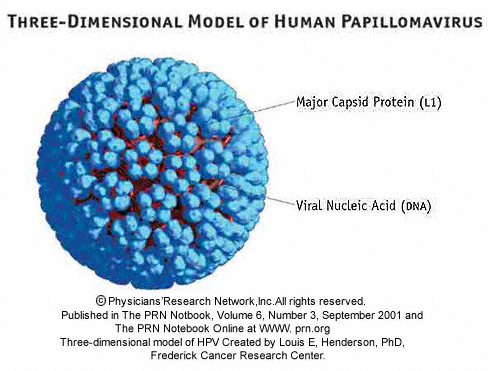
A Pap smear is a screening test that allows a doctor to look at the cells at the cervix (which is the lower part of the womb) and see if there are precancerous or cancerous cells. This test is usually performed using a speculum. Abnormal Pap smears are now known to be caused by infection with the human papilloma virus (HPV). This is a sexually transmitted virus. There are a number of different strains of HPV, and the strains that are associated with causing cervical cancer have been identified. If one has HPV, most people do not progress to cervical cancer. A similar analogy would be most people who have a cold to not develop pneumonia. Out of most women who get infected with HPV, only a small number of women develop abnormal Pap smears. Out of those, a much smaller number get progressively worse Pap smears that may develop into cervical cancer after 10-15 years. Abnormal
pap smears do not affect the

pregnancy or the baby. Rarely a procedure may be necessary (colposcopy, and/or cervical biopsy) however most procedures can be postponed until after the baby is born. If there is a history of the cervix being excised, frozen (cryotherapy) or a conization procedure then a transvaginal ultrasound is recommended at around 16-20wks to confirm there is no evidence of a short cervix (cervical insufficiency).
Pap smears are graded according to the degree of abnormality. There are three different degrees: Low Grade (LGSIL), High Grade (HGSIL), and Cancer (CIS). The progression from one stage to the other occurs over a number of years. Not all cases progress from one stage to the next; most cases of LGSIL regress to normal over time with no treatment. Management of abnormal Pap smears is dependent upon the patients’ age and degree of abnormality. Colposcopy is performed to rule out the presence of more abnormal cervical cells after an abnormal Pap smear. This procedure is performed using a specific magnifying apparatus, the cervix is carefully examined to ensure there is no evidence of cervical cancer. During this procedure cervical biopsies are often taken. In pregnancy, if necessary colposcopy and biopsies are safe.
LGSIL in a younger patient is managed expectantly with follow up pap smears and colposcopy as opposed to older patients.

Pap smears used to be reviewed by pathologist who based their diagnosis of the abnormal cells in the cervical smear, but with the knowledge that HPV is causative, most pap smears include testing to detect the presence of HPV. Newer tests can detect HPV from a urinalysis; these tests may ultimately replace the Pap smear as a screening test.
How do Abnormal Pap Smears Affect the Pregnancy and Baby?
HPV is not believed to harm the baby, or affect the pregnancy adversely. In rare cases of genital warts (also caused by HPV), a patient may have a large growth of warts called condyloma accuminata. This growth occurs in the vagina, the vuvla, or the rectum. These growths are very delicate, and during vaginal delivery can easily bleed because of the trauma of childbirth. There is a small chance the baby may be exposed to the virus. The baby has a small chance of developing a rare condition called laryngeal papillomatosis.
In some patients, the abnormal Pap smear may progress from LGSIL to HGSIL (slightly abnormal, to very abnormal). Depending upon the age of the patient, and the length of time the the abnormal Pap smear has been present, some patients may undergo a procedure called a LEEP (loop electrosurgical excisional procedure). This procedure is diagnostic, and curative. Using an “electric” knife, the abnormal portion of the cervix is removed. After this procedure usually Pap smears are performed every 4 months for one year to confirm no abnormal cervical cells were left behind. One risk of this procedure is that the amount of cervix removed may impact the ability to carry a baby to term and result in a insufficient (incompetent ) cervix. If you have had this procedure, you will need transvaginal ultrasounds around 16-20 weeks, and if your cervical length is less than 1.5cm, you may benefit from a cervical cerclage.
This procedure is rarely performed during pregnancy. If you are found to be at significant risk for cervical cancer and are pregnant, your doctor will send you to a Gyn-oncologist for their recommendations.
Website: http://www.acog.org/publications/patient_education/bp161.cfm
For more helpful pregnancy hints, instructional pregnancy videos, upcoming podcasts and to get more information about the world’s first non-toxic makeup exclusively for pregnant women, please go to www.VSACHARMD.com.