Hypothyroidism in Pregnancy
There are two types of thyroid disease, too much (hyperthyroidism) or too little (hypothyroidism). Both are clinically important, this blog post is about hypothyroidism.
Hypothyroidism in pregnancy is difficult to diagnose clinically. The symptoms of hypothyroidism are the same symptoms of pregnancy: lethargy, fatigue, difficulty sleeping, constipation, anxiety, cold intolerance, loss of hair, weight gain…every pregnant woman can tell you she has had these exact symptoms the minute she found out she was pregnant. I tell my patients that Thyroid gland is like your car’s RPM gage: if it is too low, the engine can’t work, it “sputters” along, acts like there is no gas, and you develop all the clinical symptoms of weight gain, lethargy, etc. If the Thyroid gland is working too hard (hyperthyroidism) then you have the opposite, the RPM gage is in the red zone…clinically there is weight loss, hyperactivity, your heart pumps too fast…
The diagnosis of hypothyroidism can be determined by combining the clinical findings, with a physical exam and blood tests. Some women may have an enlarged thyroid (goiter) that can be palpated by your physician during a physical exam, or you may notice that the area around your “adams” apple is a little larger.
Checking blood tests that include a TSH, FreeT4, can help confirm the diagnosis.
Why is Thyroid Important in Pregnancy?
Thyroid affects both the mother and the baby during pregnancy.
Hypothyroidism is associated with infertility, pre-eclampsia, placental abruption, miscarriage, preterm delivery, low fetal birthweight, and even fetal demise.
Your baby doesn’t make its own thyroid until about week 18-20. Until that time they are entirely dependent upon maternal thyroid. Mothers with Free T4 levels that were extremely low (hypothyroidism) had babies with a high incidence of impaired psychomotor function, and significantly lower IQ.
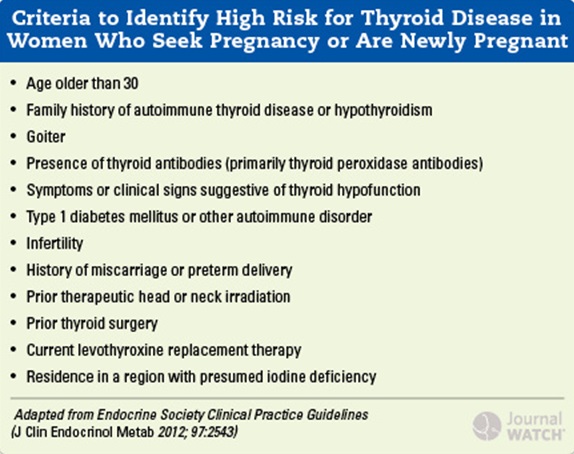
Screening
Currently ACOG does NOT recommend screening for thyroid disease in low risk women. ACOG issues recommendations, and they don’t always need to be followed. I personally feel the cost of checking for thyroid disease is so low, that it everywoman should be screened! Also, I think thyroid TSH numbers are like cholesterol numbers; most people know their exact number of their cholesterol. You should know your TSH; the goal in pregnancy (and outside of pregnancy too) is less than 2.5. If you TSH is greater than this, then you need to have your FT4 level checked, and that can give a gage of how your thyroid is functioning. If it is low, your brain is telling your thyroid gland to increase production, but your thyroid gland cannot do it, and you need supplemental thyroid.
If your TSH is low, very low for instance less than 0.05, and your FT4 is high, then your brain is telling your thyroid gland to slow down, production, and you may have hyperthyroidism.
In general the TSH and the FT4 should be checked together.
There is an instance in which you have an elevated TSH, and a normal FT4, this is called subclinical hypothyroidism. In this situation, your brain is sensing that you need more thyroid and is telling the gland to increase production, but the gland can’t go above what it is making. Eventually, the gland will “burn out” and the FT4 will go down. Some women are symptomatic with subclinical hypothyroidism. In pregnancy, any TSH greater than 2.5 is abnormal, and should be treated with supplemental thyroid. The most common cause of hypothyroidism is Hashimoto’s thyroiditis. This is a disease where your body confuses the thyroid gland as an “enemy” and makes antibodies against it (Thyroid Peroxidase Antibody, TPO). The reason this occurs is not entirely known; it may occur after a virus, where the body thinks the virus resembles the thyroid gland, so it attacks it, and it may occur after childbirth because of immune phenomenon where some fetal cells may go to the thyroid, and the moms blood attacks it.
Treatment
The goal of treatment is to keep the TSH less than 2.0-2.5, and FT4 in the upper third of normal. The usual medicaltion used is Levothyroxine, and the dose is about 0.1mcg/kg (so if you weigh about 150, that is about 70kg, so the treatment is about 70 mcg/day levothyroxine). Once you start a new treatment, it takes about 4 weeks to see a change in the TSH. TSH and FT4 levels should be followed 4 weeks after to confirm the treatment is correct. In pregnancy the TSH/FT4 should be checked about once/trimester to confirm that treatment is adequate.
In women with pre-existing hypothyroidism, the general rule is that they will need about 50% more medication during pregnancy. Taking your prenatal vitamin with levothyroxine is not recommended as it interferes with thyroxine absorption. They should be spaced apart by 2-3 hours. I usually tell women to take their prenatal vitamin at night, so that they don’t get nauseous during the day (I tried the pill once to see, and yes it made me nauseous too!). One under-recognized disorder, is Iodine deficiency. Your body needs iodine to make thyroid; it’s a building block. In pregnancy the recommended dose is about 250-300 mcg/day. Most prenatal vitamins do NOT have any iodine. Furthermore, salt is “iodized”, to give people a source of iodine, but most people try to stay away from salt because of blood pressure issues etc. It is known that 10-15% of pregnant women in the US have low iodine levels, and need supplementation. If you are unsure, get your level checked, and get a prenatal vitamin with iodine; before making any changes to your healthcare, always discuss it with your obstetrician/doctor.
After delivery, you may return to your pre-pregnancy levothyroxine dose, if you were never on any medications, discuss this with your obstetrician/doctor and they will assess if you need to continue treatment, and if so the appropriate dose. During pregnancy, the dose needed to treat hypothyroidism is always elevated compared to what you need outside of pregnancy, so dose adjustment is important.
This blog post is brought to you by www.VSacharMD.com the world’s first and only non-toxic cosmetic company dedicated to pregnancy. Created by a high risk pregnancy physician who realized that toxins in our environment, food, and daily use products can be harmful to the baby. We created this company to give women a safe cosmeticalternative during, before and after their pregnancy.
Copyright V.Sachar MD 2014. All Rights Reserved.
No part of this may be reproduced without expressed approval from the author.
This blogpost is not to be considered medical advice and is for entertainment purposes only, consult your personal
doctor before making any changes to your health care regimen.